All published articles of this journal are available on ScienceDirect.
Evaluating the Role of Serum C-Reactive Protein as a Biomarker among Patients with Chronic Obstructive Pulmonary Disease: A Cross-Sectional Study
Abstract
Background
Chronic obstructive pulmonary disease (COPD) is a multi-component systemic disease with elevated serum C-reactive protein (CRP) levels in stable conditions and during exacerbations. Serum CRP is an important biomarker and increased CRP levels lead to diminished lung function, decreased stamina to exercise, and poor quality of life in COPD patients.
Aim
This study aimed to determine the relationship between serum CRP levels and the impact of various risk factors and associated morbidities among patients with COPD attending a tertiary care hospital in Bhubaneswar.
Methods
205 stable COPD patients were enrolled. The CRP levels were analyzed with reference to the patients’ sociodemographics, clinical profiles, symptoms, and risk factors.
Results
In our study, more males were enrolled. It was observed that most of them were in the age group of 51-60 years, residing in urban areas, and belonging to a lower socio-economic group living in houses with no proper ventilation. A significant proportion of COPD patients had exposure to smoke, biomass, or dust for 20 years or more. There was no significant difference in age distribution and socio-economic status across genders. Urban slums (p = 0.048), illiteracy (p < 0.0001), ventilation status (p = 0.0009), and exposure to tobacco, smokeless tobacco, dust, etc. (p < 0.00001), were significant factors. 73% of male and 59% of female COPD patients were taking both oral and inhaler medicines. The majority of COPD patients had normal BMI. Females had a higher prevalence of wheezing symptoms (p < 0.00001), obesity (BMI ≥ 30.0), pre-diabetes (p = 0.044), and diabetes (p = 0.0200). 13% of male COPD patients had hypertension. 55% of the COPD patients had 3-10 mg/L of serum CRP, and 81% were in stage 1, 12% in stage 2, and 6% in stage 3 (GOLD). No significant gender difference in GOLD stage, duration of COPD, medication type, and hospitalization rates was observed. A higher proportion of males exhibited night/morning cough and an FEV1/FVC ratio of less than 70% predicted value. The differences in CRP levels across stages were statistically significant. The findings have provided valuable insights into the inflammatory status of COPD patients based on CRP levels, varying symptomatology, and lung function impairment.
Conclusion
COPD patients, in general, have increased levels of CRP; this emphasizes the measurement of CRP in stable COPD patients.
1. INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a significant community health problem in several countries and is likely to be the fifth reason for debilitation and the third major reason for mortality worldwide by 2030. It caused 3.23 million deaths in 2019 [1-3]. COPD is characterized by an unusual inflammatory reaction of the lung to toxic gases and debris and is distinguished by partly irreparable blockage of the airways with a decrease in airflow, which intensifies with disease progression. In India, about 30 million people suffer from COPD and COPD-associated deaths by nearly four times as compared to infectious diseases [4, 5]. Patients with chronic COPD exhibit modified lung defenses and often have multiple co-morbidities, including chronic anemia, metabolic syndrome, diabetes, cardiovascular disease, osteoporosis, depression, skeletomuscular disorders, pulmonary malignant tumors, and obstructive sleep apnea, all of which significantly influence the quality of life, frequency of exacerbation, and endurance, and determine the outcome [6]. A chronic progressive disease, like COPD, reduces the lifespan and involves increased medical expenses among the affected population. Outdoor air pollution (dust, traffic, bio-mass smoke), old age, asthma, occupational exposure, frequent respiratory tract infections during infancy, pulmonary tuberculosis, and lower socio-economic status are some of the risk factors for COPD [7]. Improving indoor and outdoor air quality can restrict the occurrence of COPD by decreasing exposure to risk factors. More medicines and longer hospitalization are required for those who have intermittent acute worsening. Various biomarkers play an important role in assessing the prognosis of COPD.
COPD is a multi-component systemic disease with elevated serum C-reactive protein (CRP) levels in stable conditions and during exacerbations. It is one of the most studied biomarkers that has been evaluated in different settings of COPD patients in order to establish a possible association with basal systemic inflammation in the stable period, cardiovascular risk events, disease prognosis, and identification of infectious exacerbations.
Systemic inflammation and increased CRP levels are correlated with diminished lung function, decreased stamina to exercise, and poor quality of life of COPD patients [7-9]. They also reflect disease severity, outcome, hospitalization, and mortality in patients with chronic respiratory failure [10-12]. Increased levels of CRP signal cardiovascular risk in COPD patients and can be treated with corticosteroids, statins, and exercise [13-17]. The levels of serum CRP in COPD patients can predict exacerbations and may accurately guide therapeutic interventions for patients with a high risk of mortality.
In an earlier study, we estimated the prevalence, risk factors, and morbidities of type 2 diabetes among patients with COPD [18]. Subsequently, the role of biomarkers and cytokines has been explored in the same cohort of COPD patients.
This study was carried out to determine the relationship between serum CRP levels and the impact of risk factors and associated morbidities, like hypertension and diabetes mellitus, among patients with COPD attending a tertiary care hospital in Bhubaneswar. Fig. (1) presents the flowchart of the methodology.
2. MATERIALS AND METHODS
2.1. Study Design
This descriptive-analytical cross-sectional study was carried out among COPD patients attending a tertiary care hospital in Bhubaneswar between December, 2021, and June, 2022. 3150 patients attending the OPD of the Department of TB & Chest Diseases at Capital Hospital, Bhubaneswar, were screened. Out of these, 2945 (93.5%) were having other respiratory diseases and/or complications not related to COPD. Patients with asthma, other chronic respiratory diseases, active pulmonary tuberculosis, malignancy, serious comorbidities, and patients using systemic corticosteroids in the preceding 3 months were excluded from the study. Pulmonary function tests (PFTs) were carried out for 274 subjects, but 69 were excluded as the PFT results were normal. Thus, 205 COPD patients diagnosed on the basis of the Global Initiative for Chronic Obstructive Pulmonary Disease (GOLD) guidelines, history, clinical examination, and PFT results were included in the study Fig. (1).
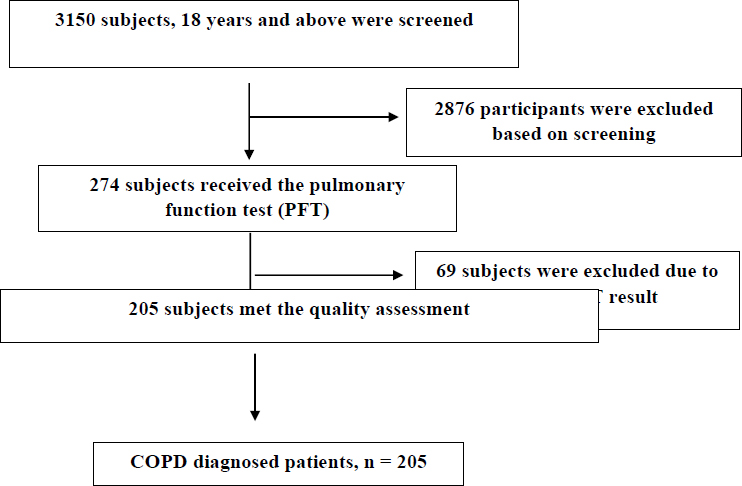
Flowchart of the methodology.
2.2. Data Collection
As part of the survey, information on age, gender, locality, socio-economic status, literacy status, occupation, body mass index (BMI), family history of asthma, mode of cooking, ventilation, exposure to smoke, dust, etc., was collected. For BMI, the height and weight of the participants were measured using an adult portable stadiometer and digital weighing scale (Dr. Morepen), respectively, after removing footwear and any other accessories. Waist circumference was measured using a measuring tape in a relaxed state after expiration. Blood pressure and blood glucose levels were measured with a digital sphygmomanometer (BP Seven, Dr. Morepen BP09) and glucometer (Gluco One, Dr Morepen BG03), respectively. Physical checkup, routine blood tests, spirometry, chest X-ray, etc., were carried out for clinical assessment. Biomass exposure was considered positive in those who lived in rural areas and regularly used wood, dung, crop residues, and coal for the purpose of cooking. Pulmonary physician in the hospital evaluated patients for COPD diagnosis. All participants were clinically stable, with no exacerbations. The criteria for stability included the absence of one or more of the three basic signs: dyspnea, sputum production, and sputum purulence. Patients having a post-bronchodilator forced expiratory volume in one second (FEV1)/forced vital capacity (FVC) <70% after inhalation of 400 mg of salbutamol were enrolled in the study. Spirometry was performed using a spirometer (Romsons, Romsons Medicons, Agra). Oxygen saturation (SpO2) in COPD patients was checked with a fingertip pulse oximeter (Everycom Electronics). Staging of COPD was done on the basis of post-bronchodilator FEV1% predicted as per the GOLD (Global Initiative for Chronic Obstructive Lung Disease) criteria. Pulmonary function tests and reversibility tests were carried out for all patients to detect airway obstruction and exclude reversible cases. The assessment of dyspnea and 6-minute walk test were performed using the modified Medical Research Council (mMRC) dyspnea scale and BODE (body mass index, airflow obstruction, dyspnea, and exercise capacity) index scores were calculated accordingly [19-21].
2.3. Methods
5 ml blood samples were collected by ante-cubital venipuncture from 205 COPD patients enrolled in the study. Serum samples obtained after centrifugation were stored at -20°C for further processing and analysis of several parameters.
2.4. Measurement of Serum CRP Levels
The measurement of serum CRP levels was performed using CRP kits (Erba Mannheim, XL System Packs, Transasia Biomedicals Ltd., Sikkim) and ERBA EM360 (fully automated clinical chemistry analyzer) as per the manufacturers’ instructions within a measuring range of 0.2-6.5 mg/dl.
2.5. Statistical Analysis
IBM SPSS version 25 was used for the analysis of the results. The prevalence has been reported with 95% confidence intervals with reference to the design effect. For each of the study's variables, descriptive statistics were analyzed. In order to evaluate the correlations between COPD and categorical independent variables, such as demographics, risk behaviours, and individual medical history, Pearson Chi-Square (χ2) test and binary logistic regression were utilized. p< 0.05 was considered as the cut-off for statistical significance.
3. RESULTS
In this study, 205 patients with COPD attending the TB & Chest Department of Capital Hospital, Bhubaneswar, were enrolled in the study on the basis of clinical examination, mecical history, PFT, and screening for CRP. The sociodemographic profile of COPD patients is depicted in Table 1. 84% (173) of the patients were male and 15% (32) were female. 31% (55) of males and 40% (13) of females were in the age group of 51-60 years. 53% (92) of males and 28% (9) of females were in the age range above 61 years. There was no significant difference in age distribution between males and females (p = 0.083). 15% (5) of the females were overweight and obese, whereas 3% (6) of males were obese. Being overweight or obese is a significant risk factor for COPD. Most patients fell into the normal BMI range (18.5-24.9). Females had a slightly higher prevalence of obesity (BMI ≥ 30.0) compared to males (p = 0.011). About 80% (137) of males and 68% (22) of females were residing in urban areas. Urban areas have a higher proportion of COPD patients. Urban slums show a notable prevalence as well (p = 0.048). Most patients were married, with no significant gender difference. 31% (54) of males and 40% (13) of females had primary education, whereas 43% (75) of males and 9% (3) of females had studied up to graduation. Illiterate patients were more prevalent among females (p < 0.0001). Graduation and higher education were more common among males. 81% (26) of females were homemakers and 78% (136) of males did not have any specified jobs. Homemakers constituted a significant portion of female patients. Government workers were more prevalent among males (p < 0.00001). With regards to socio-economic status, 42% (73) of males and 34% (110) of females were of lower economic group. No substantial gender differences were found in the socio-economic status. The risk factors associated with COPD are presented in Table 2. This table summarizes the risk factors among male and female COPD patients, including family history of asthma, cooking practices, ventilation status, and exposure to tobacco smoke, smokeless tobacco, dust, etc. The p-values indicate the significance of the differences observed between males and females for each risk factor. 31% (10) of females and 35% (96) of males were having a family history of asthma and/or COPD. Approximately 35.5% of males and 31.2% of females had a family history of asthma. No significant gender difference was observed (p = 0.117). Most of the COPD patients had indoor cooking facilities, but 75% (131) of males and 46% (15) of females were living in houses with no proper ventilation. Indoor cooking was prevalent among both males (95.4%) and females (87.5%). A small proportion of patients cooked outdoors or used a combination of indoor and outdoor methods (p = 0.169). Only 24.2% of males and 53.1% of females had proper ventilation, and the difference was statistically significant (p = 0.0009). 61% (107) of male and 31% (10) of female COPD patients had exposure to smoke, biomass, or dust for 20 years or more. Most patients (both genders) have been exposed for 20-39 years. Exposure for 1-19 years was more common among males (25.4%) than females (12.5%); however, long-term exposure (more than 40 years) was rare among the patient population. Notably, 53.12% of females reported no exposure (p < 0.00001). The clinical profile of COPD patients is depicted in Table 3. This table summarizes the clinical profile of male and female COPD patients, including GOLD stage, medication use, duration of COPD, hospitalization history, other complications, glycaemia status, and duration of diabetes. The p-values indicate the significance of the differences observed between males and females for each parameter. 26% (45) of males and 31% (10) of females were having COPD for more than 5 years. All the patients were receiving medications, i.e., inhalers (salbutamol, budesonide) and tablets (montelukast, levocetirizine, cefadroxil) from the government hospital. The majority used oral/inhaler medications. No substantial gender differences in medication type were observed (p = 0.355). A few also needed nebulization and oxygen therapy upon first visit/admission, while corticosteroids were prescribed for inflammatory reactions. 73% (127) of male and 59% (19) of female COPD patients were taking both oral and inhaler medicines. 16% (28) of male and 28% (9) of female COPD patients were hospitalized for exacerbations. Over 70% of patients had COPD for less than 5 years. No significant gender difference was, however, observed (p = 0.538). Hospitalization rates were similar between males and females (p = 0.106). Most patients had normal glycaemia. Females had a slightly higher prevalence of pre-diabetes (p = 0.044), while 1% (3) of male and 9% (3) of female COPD patients had diabetes. Diabetes was more prevalent among females (p = 0.0200) and few patients had diabetes for more than 5 years. 13% (23) of male COPD patients had hypertension, while 4% (8) of male and 3% (1) of female patients were also having TB. Hypertension and tuberculosis showed minimal gender differences. For the determination of hyperglycemia or diabetes, the blood samples were tested by a glucometer using a finger prick. With regards to the glycemic status of COPD patients, 87% (180) had normal fasting blood glucose (FBG), 2% (6) had diabetes, and 8% (15) of the male and 12% (4) of female COPD patients were having pre-diabetes. An individual was categorized as having diabetes if having an initial diabetes-related diagnosis and a strolling visit or hospitalization within the ensuing year. Table 4 depicts the symptoms of COPD patients. Among the various presenting symptoms, 46% (15) of female COPD patients were having wheezing, and chest tightness on dust exposure was experienced by 34% of the patients (11). Only 10.4% of males experienced wheezing, while a higher proportion (46.8%) of females reported this symptom (p < 0.00001). Symptoms of wheezing are a significant risk factor in COPD patients, leading to hospitalization. Cough with phlegm for more than 3 months showed similar prevalence in both genders. Fatigue was more common among females (9.3%) than males (4.6%). 45% (79) of males suffered from constant cough in the morning/night and 28% (49) experienced chest tightness on dust exposure. However, no significant gender difference in chest tightness on dust exposure was observed. With reference to the pulmonary function test, 50% of male COPD patients had <70% predicted values, whereas 46% (15) of female COPD patients had <70% FEV1/FVC and < 50% FEV1 predicted values. The FEV and FVC were much less than that in normal healthy individuals. A higher proportion of males (50.2%) had FEV1/FVC < 70% predicted values compared to females (31.2%) (p = 0.009). A similar prevalence of FEV1/FVC < 70% and FEV1 < 80% predicted values was observed in both genders. More females (46.8%) had FEV1/FVC < 70% and FEV1 < 50% predicted values than males (21.3%). These findings highlighted the varying symptomatology and lung function impairment in COPD patients. X2 value for all parameters was 9.395 (p<0.009). These findings also highlighted gender differences in the prevalence of symptoms and pulmonary function impairment among COPD patients. 21% (45) of males and 6% (14) of females suffered from exacerbations at the time of their first visit to the hospital. Table 5 shows the CRP levels in COPD patients. This table summarizes the CRP levels among COPD patients categorized by GOLD stages. The p-value indicates the significance of the differences observed between the different stages for each CRP level. CRP levels less than 3 mg/L were most common in patients (81 in total). With regard to the distribution across stages, 77 patients were in stage 1, 3 patients in stage 2, and 1 patient in stage 3. The differences in CRP levels across stages were statistically significant (p = 0.0001). A total of 113 patients had intermediate CRP levels (3 mg/L-10 mg/L). The distribution across stages was not specified. A smaller group of patients (11 in total) had higher CRP levels (10 mg/L-100 mg/L). Further, 167 patients were in stage 1, 25 in stage 2, and 13 in stage 3 (GOLD). Most patients were in stage 1 (having mild COPD). No significant gender difference was, however, observed (p = 0.211). The chi-square value was 53.739 with a p-value of 0.0001, indicating a highly significant difference in CRP levels among different GOLD stages of COPD patients.
| Parameters |
Male
[n = 173 (%)] |
Female
[n = 32 (%)] |
Statistical Analysis (Χ2, p-value) |
|
|---|---|---|---|---|
| Age (in years) | 18-28 | 2 (1.15) | 1 (3.12) | 8.216, 0.083 |
| 29-39 | 3 (1.73) | 1 (3.12) | ||
| 40-50 | 21 (12.13) | 8 (25) | ||
| 51-61 | 55 (31.7) | 13 (40.62) | ||
| > 61 | 92 (53.1) | 9 (28.12) | ||
| Body mass index (BMI) | Low (<18.5) | 10 (5.78) | 4 (12.5) | 11.044, 0.011 |
| Normal (18.5-24.9) | 108 (62.4) | 18 (56.25) | ||
| Overweight (25-29.9) | 49 (28.3) | 5 (15.62) | ||
| Obese (≥30.0) | 6 (3.46) | 5 (15.62) | ||
| Locality | Urban | 137 (79.19) | 22 (68.75) | 6.070, 0.048 |
| Rural | 31 (17.9) | 6 (18.7) | ||
| Urban slums | 5 (2.8) | 4 (12.5) | ||
| Marital status | Married | 146 (84.39) | 24 (75) | 1.698, 0.427 |
| Unmarried | 3 (1.73) | 1 (3.12) | ||
| Widow | 24 (13.87) | 7 (21.8) | ||
| Literacy status | Illiterate | 21 (12.13) | 12 (37.5) | 19.728, 0.0001 |
| Primary | 54 (31.21) | 13 (40.62) | ||
| Secondary/ Higher secondary | 23 (13.2) | 4 (12.5) | ||
| Graduate and above | 75 (43.3) | 3 (9.37) | ||
| Occupation | Govt. worker | 6 (3.4) | 1(3.1) | 147.91, 0.00001 |
| Homemaker | 2 (1.1) | 26 (81.2) | ||
| Business | 29 (16.7) | 2 (6.2) | ||
|
No specified
Job/other/student |
136 (78.6) | 3 (9.3) | ||
| Socio-economic status | Upper class | 41 (23.6) | 9 (28.1) | 1.3832, 0.709 |
| Upper middle | 27 (15.6) | 7 (21.8) | ||
| Lower middle | 32 (18.49) | 5 (15.6) | ||
| Lower class | 73 (42.1) | 11 (34.3) | ||
| Parameters | Male [n = 173 (%)] |
Female [n = 32 (%)] |
Statistical Analysis (Χ2, p-value) |
|
|---|---|---|---|---|
| Family history of asthma | Yes | 96 (35.49) | 10 (31.2) | 6.355, 0.117 |
| No | 77 (44.50) | 22 (68.7) | ||
| Cooking | Indoor | 165 (95.37) | 28 (87.5) | 3.5455,0.169 |
| Outdoor | 7 (4.04) | 3 (9.37) | ||
| Indoor/Outdoor | 1 (0.57) | 1 (3.12) | ||
| Ventilation | Yes | 42 (24.22) | 17 (53.1) | 10.963, 0.0009 |
| No | 131 (75.7) | 15 (46.8) | ||
| Exposure to tobacco smoke, smokeless tobacco, dust, etc. | 1-19 years | 44 (25.4) | 4 (12.5) | 35.299, 0.00001 |
| 20-39 years | 107 (61.8) | 10 (31.2) | ||
| More than 40 years | 4 (2.31) | 1 (3.12) | ||
| No | 18 (10.40) | 17 (53.12) | ||
| Parameters | Male [n = 173 (%)] |
Female [n = 32 (%)] |
Statistical Analysis (Χ2, p-value) |
|
|---|---|---|---|---|
| GOLD stage | Stage 1 | 88 | 11 | 3.1042, 0.211 |
| Stage 2 | 70 | 18 | ||
| Stage 3 | 15 | 3 | ||
| Medications | Oral | 22 (12.71) | 5 (15.6) | 4.390, 0.355 |
| Inhaler | 19 (10.9) | 5 (15.6) | ||
| Injectable | 2 (1.1) | 1 (3.12) | ||
| Oral/Inhaler | 127 (73.4) | 19 (59.37) | ||
| No | 3 (1.73) | 2 (6.25) | ||
| Duration of COPD | < 5 years | 128 (73.9) | 22 (68.7) | 0.377, 0.538 |
| > 5 years | 45 (26.01) | 10 (31.2) | ||
| Hospitalization | Yes | 28 (16.1) | 9 (28.12) | 2.609, 0.106 |
| No | 145 (83.8) | 23 (71.8) | ||
| Any other complications | Diabetes | 3 (1.73) | 3 (9.3) | 11.664, 0.0200 |
| Hypertension | 23 (13.2) | 1 (3.12) | ||
| Tuberculosis | 8 (4.62) | 1 (3.12) | ||
| Other | 52 (30.05) | 5 (15.6) | ||
| No | 87 (50.28) | 22 (68.75) | ||
| Status of glycaemia | Normal | 155 (89.59) | 25 (78.12) | 6.218, 0.044 |
| Pre-diabetes | 15 (8.6) | 4 (12.5) | ||
| Diabetes | 3 (1.73) | 3 (9.3) | ||
| Duration of diabetes | Less than 5 years | 1 (0.5%) | 2 (6.3%) | 0. 0.666, 0.412 |
| More than 5 years | 2 (1.2%) | 1 (3.1%) | ||
| Parameters | Male [n = 173 (%)] |
Female [n = 32 (%)] |
Statistical Analysis (Χ2, p-value) |
|
|---|---|---|---|---|
| Respiratory symptoms | Wheezing | 18 (10.4) | 15 (46.8) | 36.9, 0.00001 |
| Cough at night/morning | 79 (45.6) | 1 (3.1) | ||
| Cough with phlegm for more than 3 months |
19 (10.9) | 2 (6.2) | ||
|
Chest tightness on dust
exposure |
49 (28.3) | 11 (34.3) | ||
| Fatigue | 8 (4.6) | 3 (9.3) | ||
| Pulmonary function test | FEV1/FVC < 70% predicted value | 87 (50.2) | 10 (31.2) | 9.395, 0.009 |
| FEV1/FVC < 70% and FEV1 < 80% predicted value |
49 (28.3) | 7 (21.8) | ||
| FEV1/FVC < 70% and FEV1 < 50% predicted value |
37 (21.3) | 15 (46.8) | ||
| Number of samples screened (n = 205) | GOLD stage | Total |
Statistics
(X2, p-value) |
||
|---|---|---|---|---|---|
| CRP | Stage 1 | Stage 2 | Stage 3 | ||
| < 3 mg/L | 77 | 3 | 1 | 81 | 53.739, 0.0001 |
| 3 mg/L-10 mg/L | 89 | 14 | 10 | 113 | |
| 10 mg/L-100 mg/L | 1 | 8 | 2 | 11 | |
The data suggested that as the severity of COPD (GOLD stage) increases, there is a noticeable shift in CRP levels. Stage 1 includes the majority of patients with CRP levels < 3 mg/L, while higher stages (stage 2 and stage 3) show increased levels of CRP, with a significant proportion in the 3 mg/L-10 mg/L and 10 mg/L-100 mg/L ranges. These findings provide valuable insights into the inflammatory status of COPD patients based on CRP levels.
Elevated baseline CRP levels are significantly associated with higher mortality in COPD patients. The hazard ratio (HR) for mortality was 1.53 (95% CI 1.32–1.77) when comparing the study-specific highest CRP category to the lowest category. Similar results were observed across subgroups. Studies using a cut-off value of 3 mg/L have reported a higher mortality risk. Enrolling an Asiatic population was associated with an even higher mortality risk (HR 3.51, 95% CI 1.69-7.31).
Baseline high CRP levels may serve as a prognostic marker for late mortality in COPD patients. However, further prospective controlled studies are needed to confirm these findings. Understanding the role of CRP level in COPD can inform clinical management and risk assessment.
4. DISCUSSION
In our study, 84% of males and 15% of females were enrolled. Most of them were observed to be in the age group of 51-60 years, residing in urban areas, and belonging to a lower socio-economic group. They were living in houses with no proper ventilation. 73% of male and 59% of female COPD patients were taking both oral and inhaler medicines. In our study, the majority (61.3%) of COPD patients had normal BMI, but 26% were overweight. Further, 9% of female COPD patients had diabetes, while 13% of male COPD patients had hypertension. A significant proportion of COPD patients had exposure to smoke, biomass, or dust for 20 years or more.
There was no significant difference in age distribution and socio-economic status between males and females. Females had a slightly higher prevalence of obesity (BMI ≥ 30.0). There has been noted a prevalence of COPD in urban slums (p = 0.048). Females constituted a higher prevalence of illiterate patients (p < 0.0001). The difference in ventilation status was statistically significant between the genders (p = 0.0009). 53.12% of females reported no exposure to tobacco, smokeless tobacco, dust, etc. (p < 0.00001). Further, no significant gender difference in the GOLD stage (p = 0.211), duration of COPD (p = 0.538), medication type (p = 0.355), and hospitalization rates (p = 0.106) was noted. Females had a slightly higher prevalence of pre-diabetes (p = 0.044) and diabetes (p = 0.0200). 55% of the COPD patients had 3-10 mg/L of CRP levels, and 81% were in stage 1, 12% in stage 2, and 6% in stage 3 (GOLD). 4% of male and 3% of female patients were also having TB. CRP levels were significantly higher in the GOLD subgroups. The possible causative factors of COPD severity, including indices of lung function, oxygen saturation, dyspnea score, 6-MWD, and BODE scores, were directly related to CRP levels, but not to the duration of the disease and BMI in COPD patients. The mean serum CRP levels were found to be significantly increased in severe cases presenting with acute exacerbation of COPD on the basis of the BODE stage. A higher proportion (46.8%) of females reported wheezing symptoms (p < 0.00001), while males (45.6%) were more likely to have cough at night/morning. A similar prevalence of cough with phlegm, chest tightness on dust exposure, and fatigue was observed in both genders. A higher proportion of males (50.2%) had FEV1/FVC < 70% predicted value (p = 0.009). These findings highlighted the varying symptomatology and lung function impairment in COPD patients. Hypertension and tuberculosis showed minimal gender differences. The differences in CRP levels across stages were statistically significant (p = 0.0001). These findings provided valuable insights into the inflammatory status of COPD patients based on CRP levels.
Several studies have determined the significance of CRP in COPD patients while assessing the impact of nutrition, smoking, BMI, exercise, lung function decline, etc. [22-26].
In our study, we have tried to assess the impact of risk factors, morbidities, and correlated CRP levels with GOLD stages of COPD patients. Other studies have also found systemic inflammation in stable COPD to be linked with reduced lung function, diminished endurance, 6-MWD, and mortality in patients with mild to moderate COPD and among those with chronic respiratory failure [27, 28]. CRP is a marker of decreased metabolism and distress in severe COPD patients [29, 30]. CRP levels have been found to be elevated in smokers, individuals with reduced lung function, or those with stable COPD, indicating a risk of cardiovascular mortality. These levels decrease with treatment using inhaled fluticasone, statins, and exercise [31-34]. CRP levels below 1 mg/dl are considered normal, CRP levels between 1 and 3 mg/dl indicate intermediate risk, and levels more than 3 mg/dl imply increased risk of coronary artery disease [35]. In patients having CRP levels more than 10 mg/dl, other causes of inflammation must be explored.
5. STRENGTHS AND LIMITATIONS
This study involved a few strengths and limitations. A lesser number of COPD patients were enrolled during the study period, but they were monitored by pulmonary physician. Further follow-up cohort studies with more samples are required. The CRP levels were analyzed with reference to sociodemographic characteristics, clinical profiles, symptoms, and risk factors of the patients. The patients’ compliance with treatment was assessed based on their views.
CONCLUSION
COPD patients, in general, have increased levels of CRP. Some of the most important clinical variables that predict patient outcomes are the FEV 1 and 6-min walk distance test, irrespective of the degree of airflow obstruction. A combination of clinical examination and standard investigations, along with the use of circulating levels of CRP, can be useful to manage patients with COPD and help in improving the prognosis of these patients. The findings have emphasized the measurement of CRP in stable COPD patients. Based on our results, patients with COPD should benefit from routine CRP testing. A national control program for COPD is needed in our country due to an excessively high burden of respiratory diseases [36].
AUTHORS’ CONTRIBUTIONS
S.D.: Involved in patient enrolment, documentation of sociodemographic and clinical profiles, and sample collection; G.D.: Involved in patient recruitment, examination, and treatment of COPD patients; M.B.: Involved in the laboratory analysis of samples; N.H.: Compiled the data and performed statistical analysis; T.H.: Conceptualized the idea, designed the study, and wrote and edited the article; B.G.: Reviewed the manuscript; S.P.: Facilitated the study by providing all necessary support.
LIST OF ABBREVIATIONS
| COPD | = Chronic obstructive pulmonary disease |
| CRP | = C-reactive protein |
| PFTs | = Pulmonary function tests |
| FVC | = Forced vital capacity |
| GOLD | = Global Initiative for Chronic Obstructive Lung Disease |
| FBG | = Fasting blood glucose |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The institutional human ethics committee of ICMR-RMRC, Bhubaneswar, Odisha, India reviewed and approved the study (ICMR-RMRCB/IHEC-2020/037).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee, and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Structured questionnaires were used to collect the sociodemographic and clinical data of patients with COPD after obtaining informed written consent.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
ACKNOWLEDGEMENTS
The authors thank all the COPD patients enrolled in this study.


